Prediction
A prediction is a statement about something that might happen in the future. When weather forecasters on a Monday announce that on Friday “the weather will be warm with some rain spells in the afternoon” – they’re not making a statement of fact, but a prediction of what’s likely to happen based on current conditions (e.g., temperature, windspeed, humidity).
Healthcare providers make similar predictions. They look at a patient’s current state of health, including things like their weight, blood pressure, cholesterol level, and use it to predict what health problems (such as heart disease) the patient might face in the future. In other words, prediction in healthcare involves the analysis of past and present healthcare data to predict what will happen in the future.

These types of predictions are helpful because they can inform preventative care: i.e., they can tell patients and doctors what actions the patient should take now to prevent the predicted future health problem from developing.
In the context of AI, it is not the human doctor that is making the prediction but an AI algorithm, embedded in a medical calculator or in clinical decision support software. The algorithm will make the prediction by following a process that can be thought of as a flowchart: if the patient has X health problems now, then the patient might develop Y health problems in the future. The greater the number of such prediction rules (if/then statements) the algorithm uses to make the prediction, the harder it is to understand by humans, but the more accurate the prediction is likely to be. This is why more complex multi-layered models, such as neural networks are often used for prediction tasks.
It’s important to remember that whilst these kinds of predictions are useful, they’re not always right, and they’re not guaranteed to come true. That’s why most predictions have a degree of uncertainty attached to them (e.g., we are 67% sure that a particular outcome is likely). Also, predictions rely heavily on comparisons between different patient profiles. They assume that because patients in the past with a specific health profile (e.g., similar weight, blood pressure, cholesterol level) developed specific health conditions (e.g. heart disease), it’s likely that the new patient with the same profile will also develop the same health conditions. This is not, however, a guaranteed outcome. Instead, these types of predictions describe ‘relative risk’: i.e., compared to people with lower weight, blood pressure and cholesterol, patients with higher weight, blood pressure, and cholesterol, are more likely to be at risk of developing heart disease in the future.
In the context of healthcare, prediction involves using a predictive model to estimate an individual’s risk of a specific healthcare outcome (e.g., having a particular disease now, being readmitted to hospital, or developing a specific condition in the future), by looking at the outcomes of ‘similar’ individuals in the past. The predicted ‘risk’ is not an absolute risk, but probable and relative: i.e., just because a model predicts that it is X% likely that a person with Y condition and Z characteristics will develop a particular condition in the future, that does not guarantee that the person will develop the condition.
Traditionally, such risk prediction models have been regression-based models which estimate a baseline risk and then create a linear list of covariates, different combinations of which increase or decrease the likelihood of a particular outcome (i.e., increase or decrease the frequency with which a particular outcome will occur given a particular combination of covariates).
For instance, a logistic regression model developed fairly early on in the COVID-19 pandemic was used to identify the fact that individuals with a higher BMI or from black or minority ethnic groups were at greater risk of adverse outcomes from infection (e.g., hospitalisation) compared to the ‘baseline’. Other well-known examples of regression-based risk prediction scores commonly used in medicine include the Framingham Risk Score for 10-year risk of cardiovascular disease or the Kidney Failure Risk Score for 10-year risk of end-stage kidney failure.
These traditional regression-based models are widely implemented in healthcare systems across the globe. However, there are a number of distinct disadvantages:
- they can confuse correlation and causation
- they model what increases risk (for example) but do not explain why
- they assume that the relationships between variables are always straightforward and linear
- they cannot be combined easily to identify how different outcomes (e.g., co-morbidities) interact to alter risk level
- each individual outcome of interest requires a new bespoke-trained model
- the range of variables (for example phenotypic, or genetic, or ‘clinical’) that they can handle is limited.
This is why it is increasingly common for risk-prediction models to be based on machine-learning models which are less affected by these limitations.
The exact machine learning models used in risk-prediction models depend on whether the model is being trained on structured data (such as electronic health record data) or unstructured data (such as freetext data). If it is structured data, the model is likely to be an artificial neural network. If it is unstructured data, it’s likely to be a convolutional neural network. In both instances, it is most likely that the model will incorporate Bayesian principles during training and so become a ‘Bayesian neural network’. This is because Bayesian networks are graphical models that are capable of making predictions involving joint probability (i.e., the likelihood of two or more events happening at the same time) and conditional probability (i.e., what if this one factor or variable was changed). These capabilities mean Bayesian networks can be used to generate individual-risk-level predictions that can eventually be implemented into clinical decision support software and help with tasks such as treatment planning.
An Owkin example
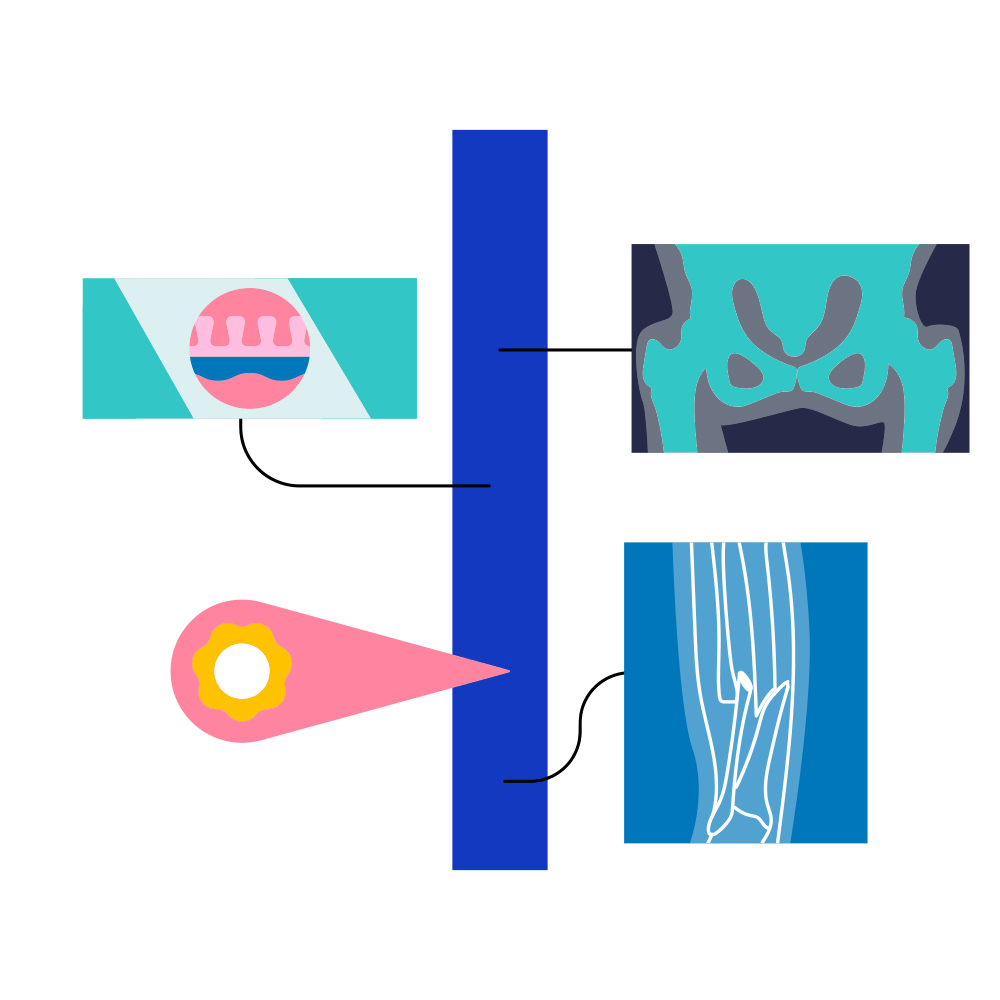
RlapsRisk BC aims to revolutionize breast cancer care management through deploying AI software to support clinicians in understanding the risk of relapse for breast cancer patients. This AI solution is trained to assess and predict the risk of distant relapse after surgery from HES pathology images (taken from a tumor).
Clinicians can use the information provided by our solution to select the best treatment for each patient. RlapsRisk BC offers comparable performance to standard molecular testing, yet relies upon more readily accessible data from surgical resections. This reduces turnaround time and democratizes access to actionable medical insights, making precision medicine more available to more patients.
Further reading
- Arora, Paul et al. 2019. ‘Bayesian Networks for Risk Prediction Using Real-World Data: A Tool for Precision Medicine’. Value in Health 22(4): 439–45.
- Balthazar, Patricia, Peter Harri, Adam Prater, and Nabile M. Safdar. 2018. ‘Protecting Your Patients’ Interests in the Era of Big Data, Artificial Intelligence, and Predictive Analytics’. Journal of the American College of Radiology15(3): 580–86.
- Bulgarelli, Lucas, Rodrigo Octávio Deliberato, and Alistair E. W. Johnson. 2020. ‘Prediction on Critically Ill Patients: The Role of “Big Data”’. Journal of Critical Care 60: 64–68.
- de Hond, Anne A. H. et al. 2022. ‘Guidelines and Quality Criteria for Artificial Intelligence-Based Prediction Models in Healthcare: A Scoping Review’. npj Digital Medicine 5(1): 2.
- Paulus, Jessica K., and David M. Kent. 2020. ‘Predictably Unequal: Understanding and Addressing Concerns That Algorithmic Clinical Prediction May Increase Health Disparities’. npj Digital Medicine 3(1): 99.